From a human perspective, there’s a lot to dislike about Shigella.
The more you learn about these infection-causing microbes, the easier it is to picture them as the dastardly, mustache-twirling villains of the microbial world.
Let’s take a quick look at Shigella’s rap sheet.
Shigella are a form of pathogenic (disease-causing) bacteria that evolved over millions of years specifically to infect humans.
Infections are primarily transmitted through contaminated food or water, but can also be transmitted through surface contact.
A shigellosis infection can cause a bad case of diarrhea, fever and stomach cramps that lasts from five to seven days. Shigella causes about 500,000 cases of diarrhea in the United States annually.
Fortunately, most of these cases resolve without causing lasting damage.

Worldwide, Shigella is a much bigger problem.
Infections are estimated to cause up to 165 million cases of disease and 600,000 deaths each year, primarily in children under the age of five in developing nations.
Plus there are new, antibiotic-resistant strains of Shigella emerging that are much more difficult to treat.
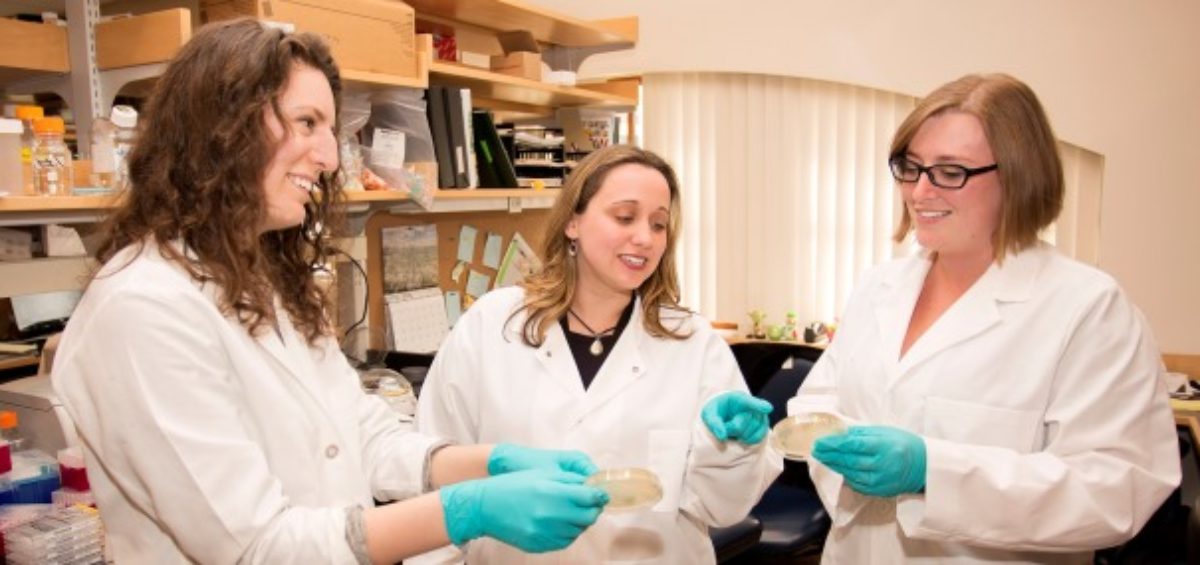
Christina Faherty, PhD, a researcher at the Mucosal Immunology and Biology Research Center at Massachusetts General Hospital for Children, is developing two new strategies for treating Shigella that could finally overcome 50 years of failed treatment efforts.
The case for a new approach
Faherty’s research team has demonstrated that Shigella undergoes a series of changes as it travels through the human digestive system, primarily as a result of exposure to bile in the small intestine.
The changes, which are driven by genes within the bacteria, help to protect it during its journey through the stomach and small intestine.
By exposing Shigella to bile salts in the lab, Faherty has identified several strategies the bacteria employs for self-preservation, including the formation of a biofilm, which provides a protective niche for bacterial cells, and the activation of a molecular efflux pump to remove bile that makes it into the bacterial cell.
Researchers have demonstrated similar bile-specific responses in other types of infectious bacteria, including Vibrio and pathogenic Escherichia coli.
From a scientific perspective, Faherty can’t help feeling a grudging admiration for these strategies, even as she works to defeat them.
“To me it seems like these pathogens have their own little brain, and they know how to manipulate the host and cause infection. It’s really interesting what they’re doing, but I want to stop them from doing it.”
The changes that Shigella undergo during their journey means that the microbes that launch their attack in the colon look a lot different from the Shigella strains that have been cultured in the laboratory. One reason for the lack of success in developing a vaccine could be that the immune system of a vaccinated individual does not recognize the bacteria following gastrointestinal transit.
Faherty hopes to create a more effective vaccine by adjusting the lab culture process to better replicate the conditions the bacteria are exposed to in the digestive system, which could hopefully prime the body to respond to the bacteria at the point of attack.
With the help of a grant from the Bill & Melinda Gates Foundation, Faherty is also collaborating with researchers at MIT to develop new bacteriophages—custom-made viruses that could be designed to infect and kill Shigella—in the intestines without harming beneficial bacteria.
The role of antibiotic resistance
Vaccines and bacteriophages could be crucial to treating shigellosis in the future, given the skyrocketing rates of antibiotic resistance. “It’s a huge problem,” Faherty says. “We are running out of antibiotics at this point.”
Faherty’s research has demonstrated that many of the mechanisms Shigella employs to resist bile are also used to resist antibiotics. “The sheer fact that they are exposed to bile on their way to the colon enhances their ability to resist certain antibiotics.”
Faherty explains that the same molecular pump Shigella uses to identify and remove bile from the bacterial cell is also used to identify and remove antibiotics.
“If you are going to design a new antibiotic, it is important to determine if the new candidate will be affected by the same mechanisms. Otherwise, resistance to this new antibiotic will quickly develop.”
“This is going to be a constant battle,” Faherty acknowledges. “Infectious bacteria have been around for millions of years, and they know what they’re doing, so we’re going to have to constantly stay ahead of them.”
About the Mass General Research Institute
Research at Massachusetts General Hospital is interwoven through more than 30 different departments, centers and institutes. Our research includes fundamental, lab-based science; clinical trials to test new drugs, devices and diagnostic tools; and community and population-based research to improve health outcomes across populations and eliminate disparities in care.
Support our Research






Leave a Comment