Study highlights the pitfalls of basing clinical recommendations on data heavily skewed towards one race or ethnic group.
Blog
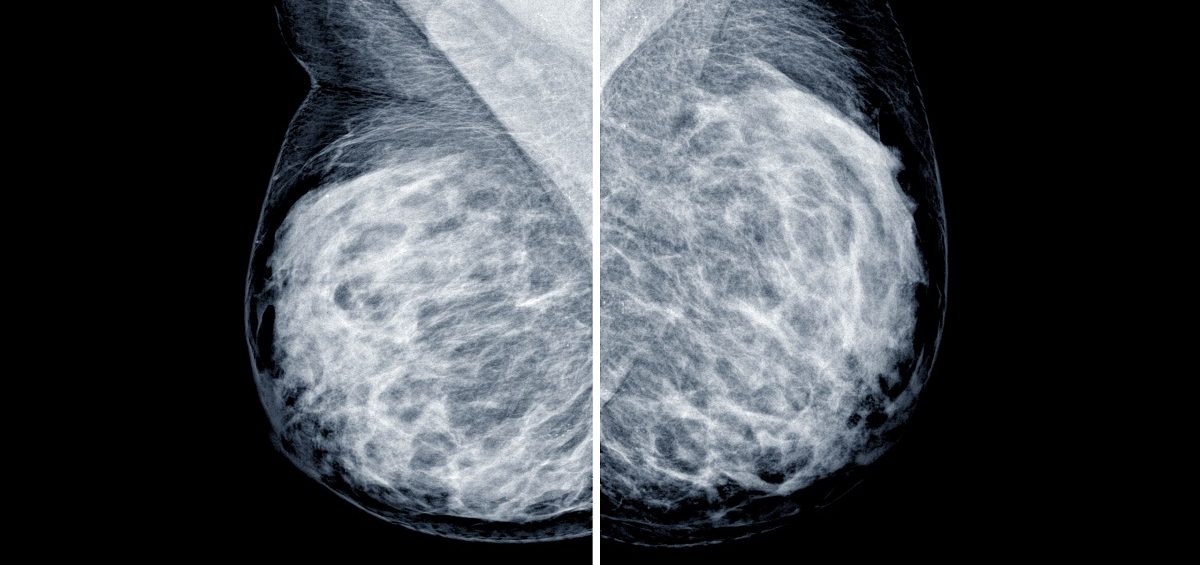
Imagine enduring a painful, expensive and scar-inducing surgery—only to find out afterwards that it wasn’t necessary. This is the situation for many women with high-risk breast lesions.