A recent study both validated time to surgery as a standardized metric for breast cancer care and identified a worrying difference in time to surgery between Black and white patients.
Blog
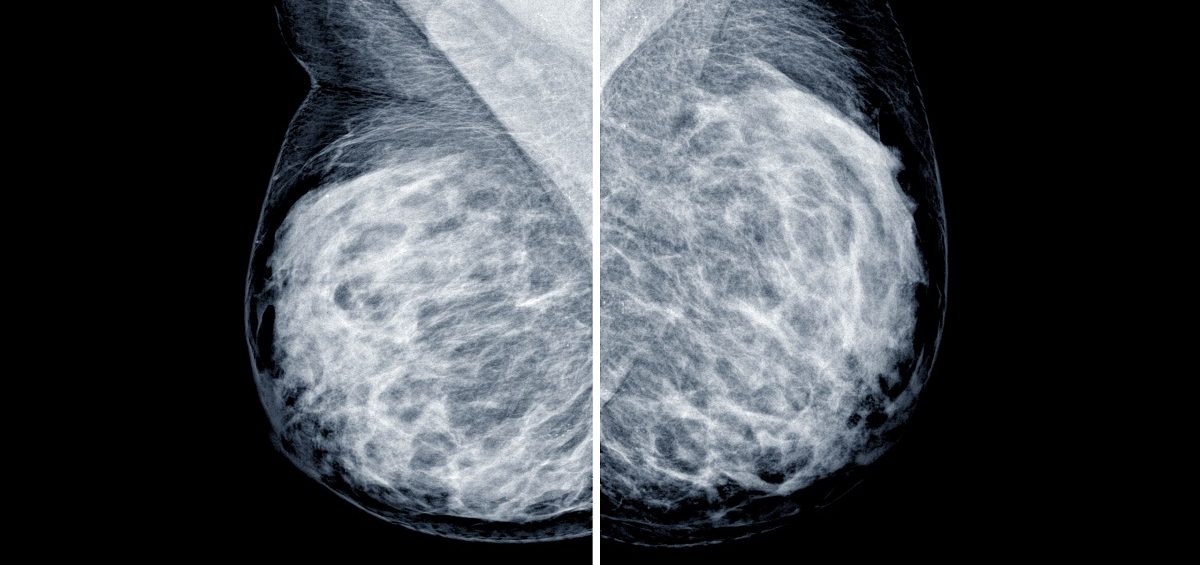
Dr. Bahl is using artificial intelligence (AI) and deep learning (DL) to improve the detection, diagnosis, and treatment of breast cancer.
Randy C. Miles, MD, MPH, and Constance Lehman, MD, PhD, recently investigated the readability of patient education content on breast density and found many resources do not meet the AMA recommendation of a sixth grade reading level.
When you love music, you go to a concert. When you love art, you go to a gallery. But when you love science you can’t just go to a laboratory — or can you?
Study highlights the pitfalls of basing clinical recommendations on data heavily skewed towards one race or ethnic group.
Imagine enduring a painful, expensive and scar-inducing surgery—only to find out afterwards that it wasn’t necessary. This is the situation for many women with high-risk breast lesions.